Hyponatremia, defined as a serum sodium concentration below 135 mEq/L, is the most common electrolyte abnormality encountered in clinical practice. Hyponatremia is a common electrolyte abnormality caused by an excess of total body water in comparison to that of the total body sodium content.
Hyponatremia represents an imbalance in this ratio where total body water is more than total body solutes. Total body water (TBW) has two main compartments, extracellular fluid (ECF), accounting for one-third, and intracellular fluid (ICF), accounting for the remaining two-thirds. Sodium is the major solute of ECF, and potassium for ICF.
It is associated with increased morbidity and mortality, particularly in hospitalized patients.
Classification of Hyponatremia
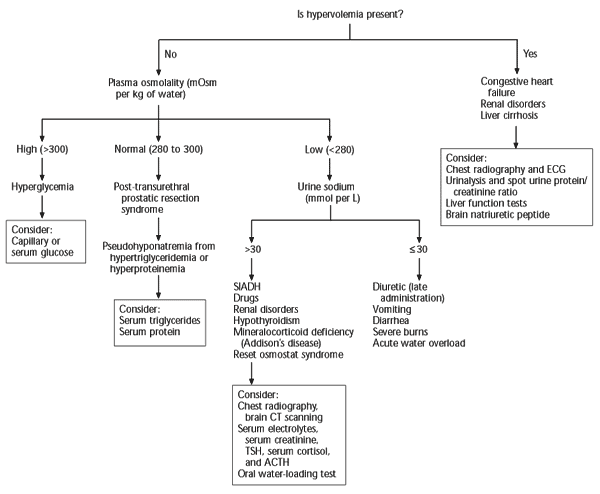
The etiology of hyponatremia can be classified based on the volume status and serum osmolality. As mentioned earlier, sodium is the major solute of extracellular fluid (ECF). Based on the volume of ECF, a patient can be classified into hypovolemic, euvolemic, or hypervolemic.
Step 1 : Check Serum Osmolality (mOsm/kg)
This distinguishes true hypotonic hyponatremia from other forms.
1. Hypotonic hyponatremia ( > 275 mOsm/kg)
→ true hyponatremia (most common and clinically relevant)
2. Isotonic hyponatremia (275 – 290 mOsm/kg)
→ pseudohyponatremia (e.g., severe hyperlipidemia/proteinemia)
3. Hypertonic hyponatremia (> 290 mOsm/kg)
→ osmotically active solutes (e.g., glucose, mannitol)
📌 Conclusion: Always start with serum osmolality. Only if hypotonic, move to volume status assessment. Next, go to step 2.
Step 2: Urine Osmolality
- Urine osmolality less than 100 mOsm/kg indicates primary polydipsia or reset osmostat.
- Urine osmolality greater than 100 mOsm/kg usually indicates a high ADH state; go to step 3.
Step 3 : Check Volume Status
Volume status becomes relevant only for hypotonic hyponatremia, and it directly guides management strategies. If serum osmolality <275 mOsm/kg, the patient has true hypotonic hyponatremia. At this point, volume status becomes the key stratifier:
1. Hypovolemic Hyponatremia
- Loss of both sodium and water; sodium loss > water loss.
- Causes:
- GI losses: vomiting, diarrhea
- Renal: diuretics, mineralocorticoid deficiency
- Skin: burns, sweat
2. Euvolemic Hyponatremia
- Increased total body water, normal sodium.
- Causes:
- SIADH
- Hypothyroidism
- Adrenal insufficiency
- Psychogenic polydipsia
3. Hypervolemic Hyponatremia
Hyponatremia in the presence of edema indicates increased total body sodium and water.
- Excess water and sodium; water gain > sodium gain, resultinbg in edema.
- Causes:
- CCF
- Liver Cirrhosis
- Renal : Nephrotic syndrome / Advanced renal failure
Step 4: Urine Sodium Concentration
- Urine sodium less than 10 mmol/L indicates extrarenal loss of fluid (remote diuretic use and remote vomiting).
- Urine sodium greater than 20 mmol/L suggests renal loss of urine (diuretics, vomiting, cortisol deficiency, and salt-wasting nephropathies).
Hyponatremia Severity Classification Table
| Severity | Serum Sodium (mEq/L) | Typical Symptoms | Clinical Implications & Management |
|---|---|---|---|
| Mild | 130–134 | Often asymptomatic, nausea, headache, mild dizziness | Monitor; treat underlying cause; consider fluid restriction if SIADH or mild chronic case |
| Moderate | 120–129 | Confusion, gait disturbance, fatigue, lethargy | Requires active management; may need fluid restriction, salt tablets, or loop diuretics |
| Severe | <120 | Vomiting, seizures, coma, respiratory arrest | Medical emergency; initiate 3% hypertonic saline (100 mL bolus), monitor sodium closely; prevent overcorrection |
Chronic hyponatremia (>48 hours) allows cerebral adaptation; hence symptoms may be milder. Thus cant correct too fast!
Diagnostic Workup
- Confirm hyponatremia and exclude pseudohyponatremia or translocational causes.
- Assess serum osmolality
- Determine volume status via clinical exam
- Urine studies:
- Urine osmolality (>100 mOsm/kg suggests impaired water excretion)
- Urine sodium (>40 mEq/L in SIADH or renal losses)
- Endocrine evaluation: TSH, cortisol
Management
Treatment of hyponatremia depends upon the degree of hyponatremia, duration of hyponatremia, severity of symptoms, and volume status.
- Acute ( < 48H) : can correct fast
- Chronic ( > 48H) : cant correct fast, because brain already adapt with that low sodium level
Acute Symptomatic Hyponatremia
- Severe: 3% hypertonic saline boluses: 100 mL over 10 minutes, may repeat up to twice if symptom persists
- Mild to moderate : 3% hypertonic saline slow infusion (use sodium deficit formula to calculate the rate of infusion but recalculate rate with frequent sodium monitoring).
Target: Increase serum sodium by 4–6 mEq/L in first 6 hours
Chronic Asymptomatic Hyponatremia
- Severe:
- Symptomatic : 3% hypertonic saline boluses: 100 mL over 10 minutes, may repeat up to 3 times.
- No symptoms : 3% hypertonic saline boluses: 50 mL over 10 minutes, may repeat up to 3 times.
- Moderate :
- Symptomatic : 3% hypertonic saline slow infusion (use sodium deficit formula to calculate the rate of infusion but recalculate rate with frequent sodium monitoring).
- No symptoms : General measures
- Mild : General measures
Avoid overcorrection: No more than 8–10 mEq/L in 24h, 18 mEq/L in 48h
In most cases of chronic asymptomatic hyponatremia, general measures involves:
- Find and treat reversible/underlying cause
- Fluid restriction (less than 1 to 1.5 L per day) is the mainstay of treatment and the preferred mode of treatment for mild to moderate SIADH
- Stop any meds that can cause hyponatremia:
- Diuretics
- Carbamazepine
- Chlorpromazine
- Vasopressin analogs
- Indapamide
- SSRI
- Theophylline
- Amiodarone
- Ecstasy
SIADH
SIADH is an important cause of hyponatremia that occurs when normal bodily control of antidiuretic hormone secretion is lost and antidiuretic hormone is secreted independently of the body’s need to conserve water. Antidiuretic hormone causes water retention, so hyponatremia then occurs as a result of inappropriately increased water retention in the presence of sodium loss.
Complications
If left untreated or inadequately treated, patients with hyponatremia can develop rhabdomyolysis, altered mental status, seizures, and even coma.
Rapid correction of chronic hyponatremia (greater than 10 mEq/L to 12 mEq/L of sodium in 24 hrs) can lead to osmotic demyelination syndrome. Presents 2–6 days post-correction with dysarthria, dysphagia, quadriparesis, “locked-in” syndrome
Special Considerations
- Elderly patients: Increased risk due to impaired renal dilution and polypharmacy
- Postoperative patients: Monitor sodium closely, especially with hypotonic IVF
- ICU patients: High incidence due to SIADH, fluid shifts, and medications
Conclusion
Hyponatremia requires careful assessment of volume status, underlying etiology, and symptom severity. Management should be individualized, avoiding both undertreatment and overly rapid correction to prevent catastrophic complications like ODS. Clinicians must be vigilant, particularly in hospitalized and critically ill patients, where hyponatremia often signifies a poor prognosis.
Hyponatremia Correction Calculator
Show formula
Na⁺ Requirement (mmol) = Total Body Water × (Desired Na⁺ − Serum Na⁺)
Infusion Rate (cc/hr) = [Na⁺ Requirement × 1000] ÷ [Infusate Na⁺ × Time (hrs)]
Total Body Water (TBW):
• Children: 0.6 × weight (kg)
• Women: 0.5 × weight (kg)
• Men: 0.6 × weight (kg)


[…] Artikel penuh -> https://notamedik.com/hyponatremia/ […]