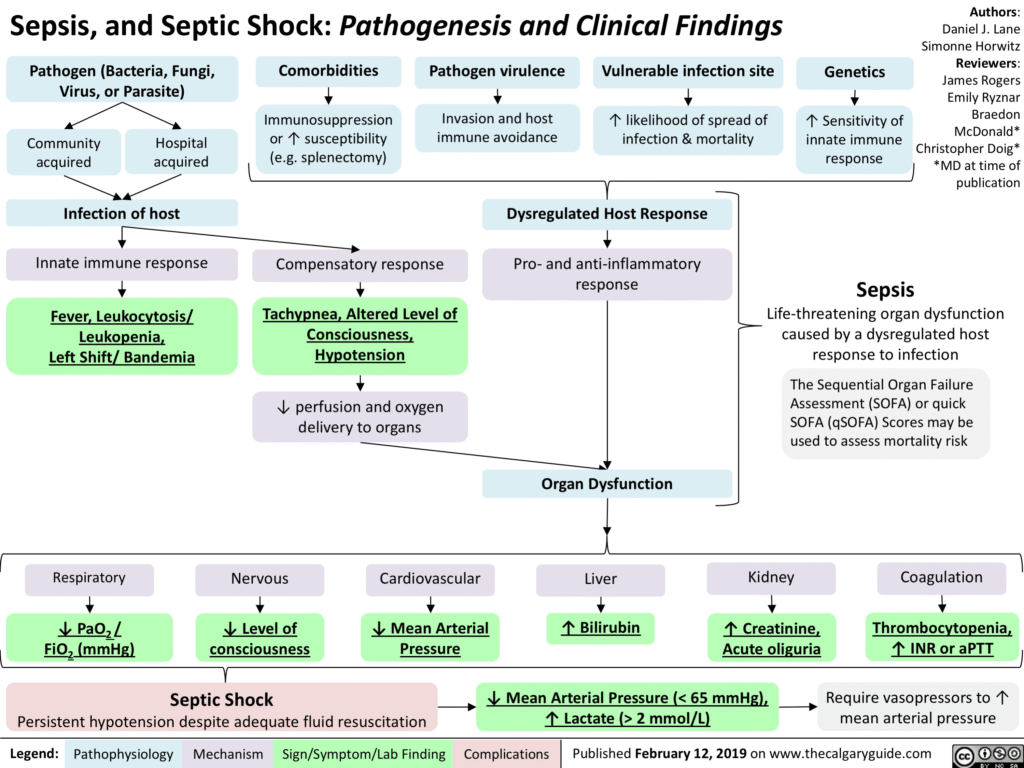
Sepsis is a life-threatening condition that occurs when the body’s response to an infection damages its own tissues and organs. It’s essentially an overreaction of the immune system to an infection, leading to widespread inflammation and potential organ failure. If left untreated, sepsis can progress to septic shock and death.
Fever
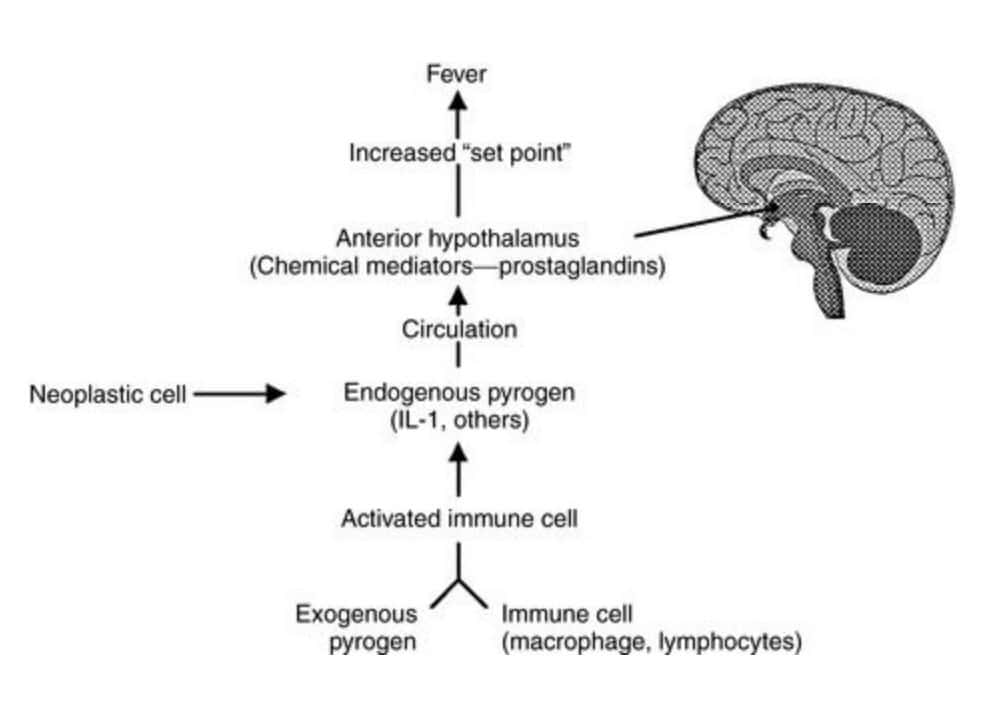
Fever is the elevation of an individual’s core body temperature above a ‘set-point’ regulated by the body’s thermoregulatory center in the hypothalamus.
This increase in the body’s ‘set-point’ temperature is often due to a physiological process brought about by infectious causes or non-infectious causes such as inflammation, malignancy, or autoimmune processes.
These processes involve the release of immunological mediators, which trigger the thermoregulatory center of the hypothalamus, leading to an increase in the body’s core temperature
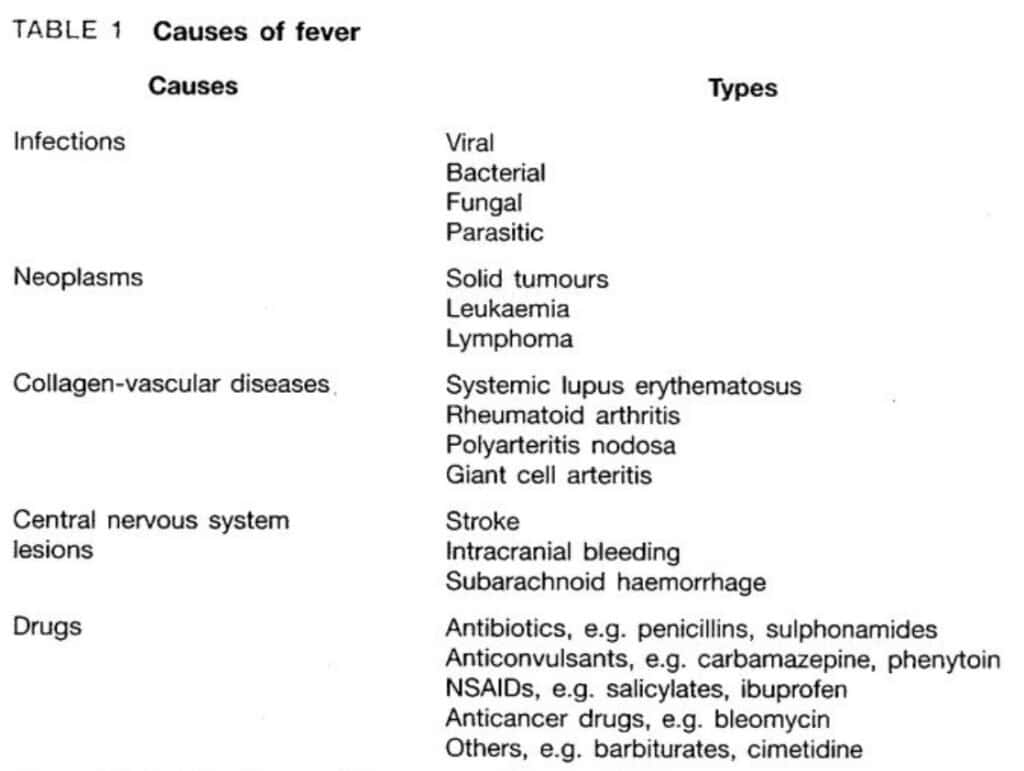
Causes Of Fever
Common Causes of Sepsis
Sepsis can be caused by bacterial, viral, fungal, or parasitic infections. The most common sources include:
- Lung infections – e.g., pneumonia
- Urinary tract infections (UTIs)
- Abdominal infections – such as appendicitis
- Skin infections or infected wounds
- Post-surgical infections
Systemic Inflammatory Response Syndrome (SIRS)
2 or more of following criteria:
- Temperature > 38℃ or < 36℃
- Heart rate > 90 bpm
- Resp. rate >20 breaths/min or PaCO2 < 4.5 kPa (32 mmHg)
- WBC >12 or < 4 x 109 /L or immature (band) neutrophil > 10%
In severe cases, sepsis can progress to:
- Severe sepsis – damage to vital organs such as the kidneys, liver, or lungs.
- Septic shock – dangerously low blood pressure that can result in death.
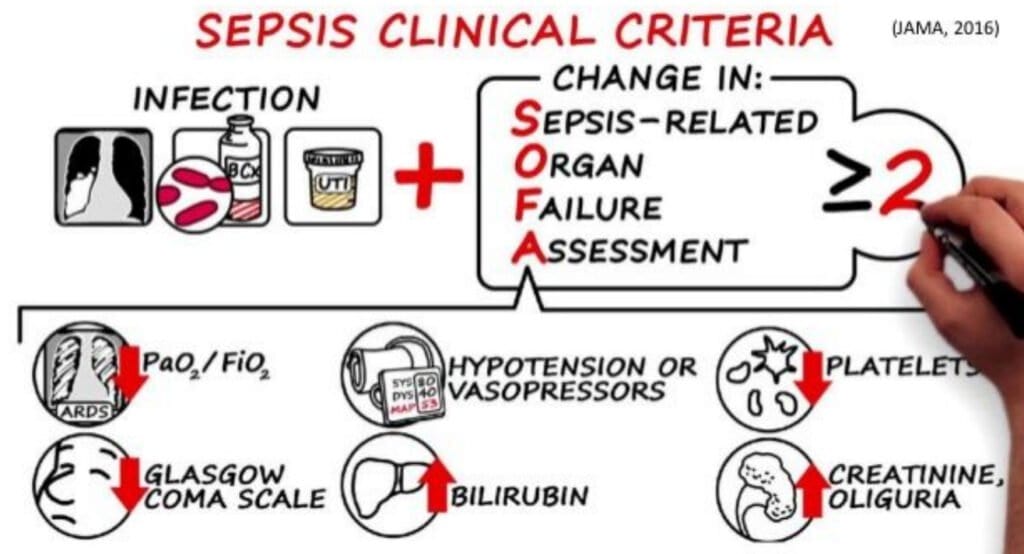
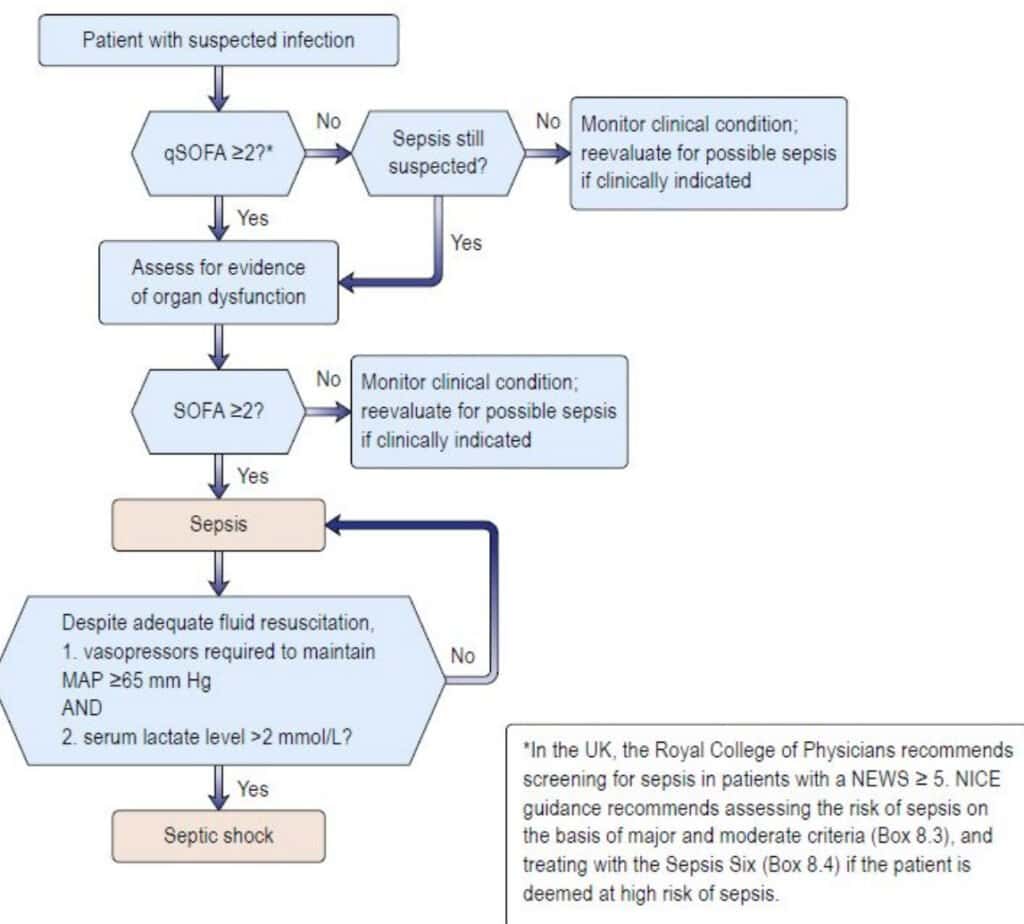
Quick SOFA (qSOFA)
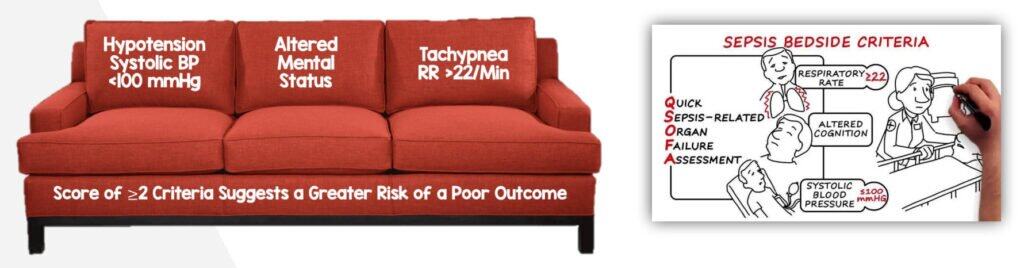
▹ Score of ≥ 2 in patient with suspected or documented infection should be assumed to have sepsis
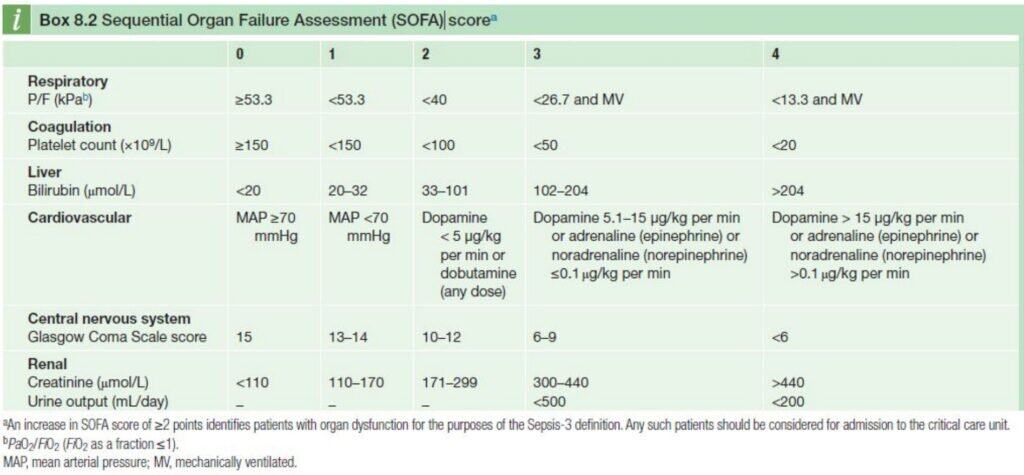
Sequential Organ Failure Assessment (SOFA)
Shock
A state of circulatory insufficiency that creates an imbalance between tissue oxygen supply (delivery) and oxygen demand (consumption) resulting in end-organ dysfunction.
How to define shock
- Hypotension
- SBP<90mmHg or MAP< 65 mmHg (May be normal in compensated state)
- MAP = [2(DBP) + SBP] / 3
- Or in chronic hypertensive patient : 40mmHg drop in SBP from baseline
- SBP<90mmHg or MAP< 65 mmHg (May be normal in compensated state)
- Refractory shock:
- Persistent hypotension with end-organ dysfunction despite fluid resuscitation,
high-dose vasopressors, oxygenation, and ventilation
- Persistent hypotension with end-organ dysfunction despite fluid resuscitation,
Septic Shock
Severe subset of sepsis where circulatory & cellular changes are associated with a substantial increase in mortality
Persistent hypotension requiring vasopressor to maintain MAP ≥ 65 mmHg & serum lactate ≥ 2 mmol/L despite adequate fluid resuscitation (¬30 mL/kg)
Signs and Symptoms of Sepsis
| Symptoms | Signs | |
|---|---|---|
| Infection/ Inflammation | Fevers, chills, rigors, sweating | Septic looking, fever, tachycardia, tachypnea |
| Hypotension | Dizziness, lightheadedness, nausea, fatigue, loss of concnetration, faint | Cold, pale peripheries CRT < 2sec Systolic BP < 100mmHg Tachycardia |
| Multiorgan failure | Respiratory – Shortness of breath Cardiovascular – hypotensive symptoms Central Nervous System – Altered mental status Gastrointestinal – intolerance with enteral feeding Renal – oliguria Liver – yellowish discolouration, pruritus Coagulation – bleeding tendency | Respiratory – tachypnea CVS – tachycardia, bounding pulse CNS – GCS drop Liver – jaundice Coagulation – bleeding tendency |
| Sources of Infection | Systemic reviews | Full examination |
Investigations
| Blood tests | Findings | Reasons |
|---|---|---|
| Full Blood Count (FBC) | Leukocytosis Thrombocytopenia | Infection DIVC (late presentation) |
| Arterial Blood Gas (ABG) | Low PaO2 High Lactate | Respiratory failure / ARDS Significant tissue hypoperfusion |
| Renal Profile Electrolytes | Urea, Creatinine raised Electrolyte imbalance | Severe dehydration or renal failure |
| Liver Function Test | Hyperbilirubinemia Increased ALP & ALT | Liver involvement |
| Coagulation profile | Increased PT & APTT | Coagulopathy / DIVC |
| Blood Culture & Sensitivity | Organism growth | Detect causative organism |
| UFEME, Urine C&S | Leukocyte, bacterial growth | Exclude UTI |
| Dextrose stick | Exclude hypoglycaemia |
Imaging
– depends on source of infection#
Chest, abdominal or extremity radiography
Abdominal ultrasonography
CT abdomen or head
Others
– Lumbar Puncture : suspected meningitis
Management
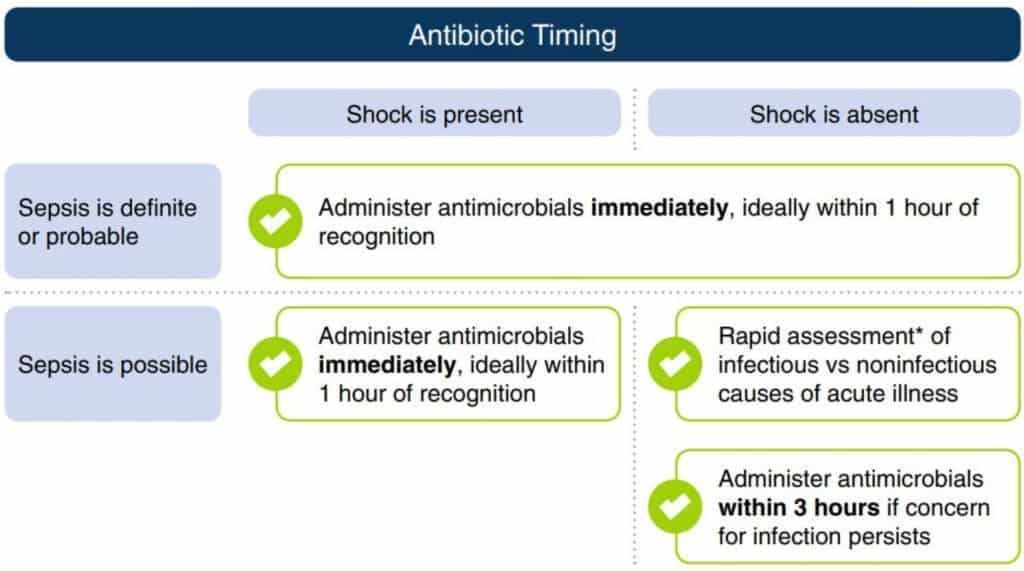
1 hour sepsis bundle
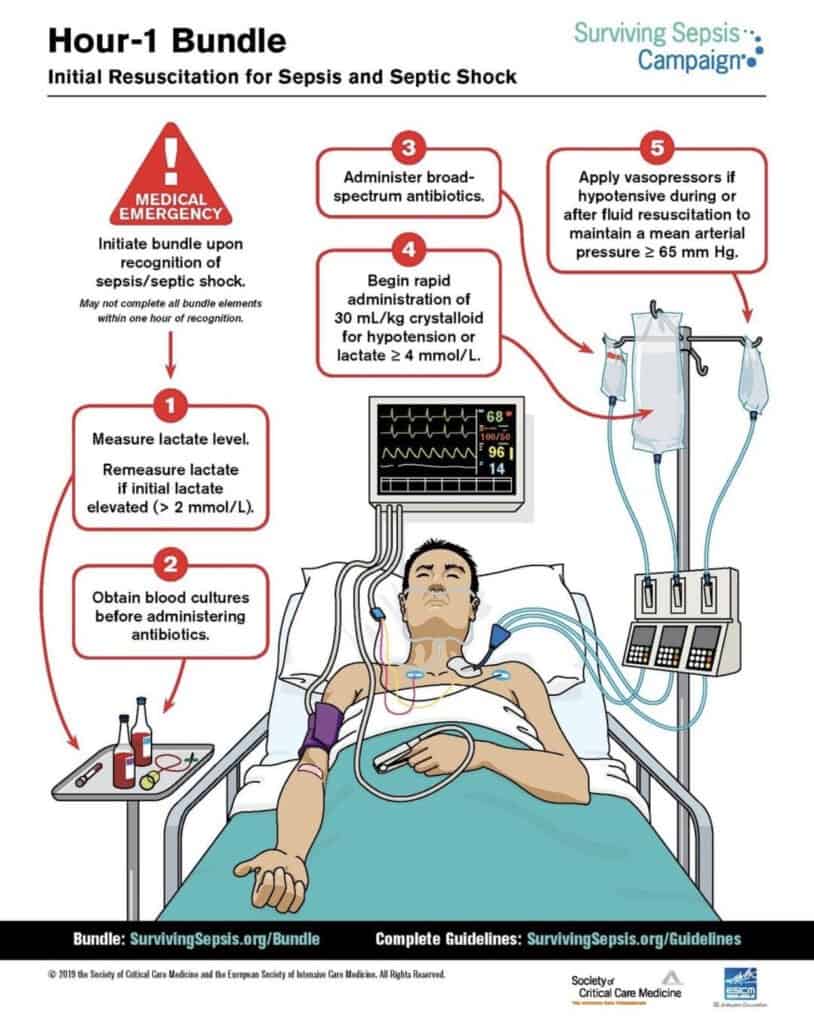
The 1-h bundle is composed of the following five elements:
- Measure lactate level.
- Taking Blood for cultures
- Broad-spectrum antibiotics.
- Fluid resuscitation with 30mL/kg crystalloid for hypotension or lactate ≥4 mmol/L.
- Starting vasopressors to maintain MAP of 65 in refractory hypotension following or during fluid resuscitation
Fluid Resuscitation
Fluid Choice (bases on SSC Guidelines)
- Crystalloids are the preferred first line fluid for resuscitation
- A balanced crystalloid is preferred over normal saline
- For adults with sepsis or septic shock, we suggest using albumin in patients who received large volumes of crystalloids over using crystalloids alone
Treatment Targets
- Systolic BP >90 mmHg.
- Normal conscious level
- Respiratory rate <25 breaths/minute
- Lactate <2 mmol/l Adequate Capillary refill time, pulse rate and urine output
When to stop or escalate therapy
- Once the patient meets the desired targets then further fluids will be prescribed if needed.
- Stop if there are signs of overload.
- If after the 30ml/kg there is inadequate BP and lactate is > 4mmol/l –> SEPTIC SHOCK
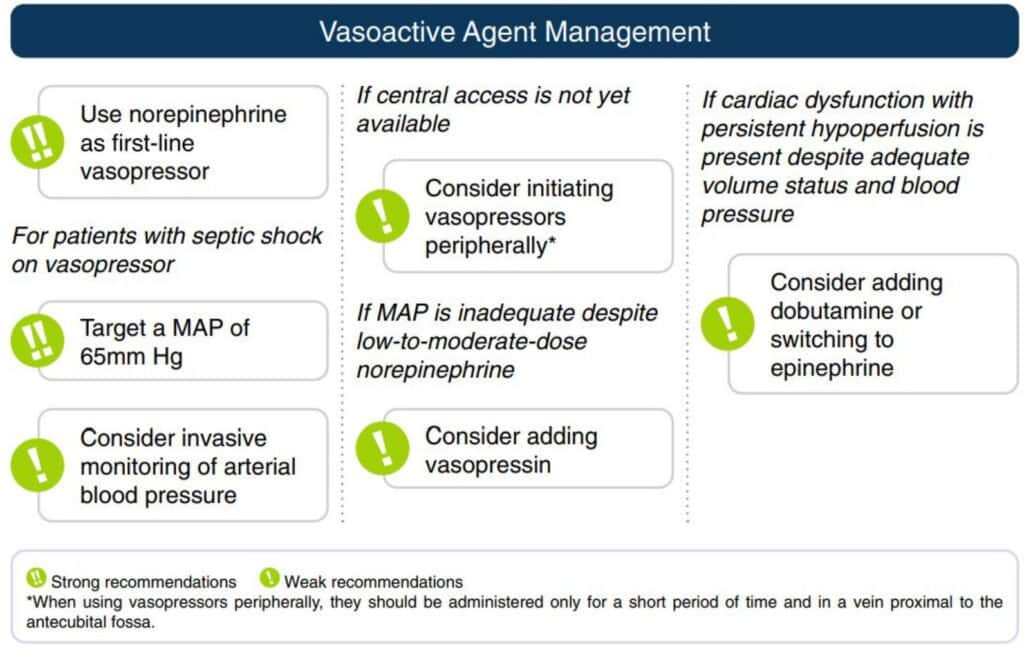
Vasopressor Management
For adults with septic shock, we recommend using norepinephrine as the first-line agent over other vasopressors
– Strong recommendation !
- Where norepinephrine is not available, epinephrine or dopamine can be used as an alternative.
- For adults with septic shock, we suggest starting vasopressors peripherally to restore MAP rather than delaying initiation until a central venous access is secured
- When using vasopressors peripherally, they should be administered only for a short period of time and in a vein in or proximal to the antecubital fossa
Who is at Risk of Developing Sepsis?
Sepsis can affect anyone, but certain groups are at higher risk:
- Infants and the elderly
- People with chronic illnesses (e.g., diabetes, kidney disease)
- Individuals with weakened immune systems (e.g., cancer or HIV patients)
- Those undergoing invasive medical procedures (e.g., catheters, intubation)
- Recent surgical patients
Frequently Asked Questions (FAQs)
Is sepsis contagious?
No, sepsis itself is not contagious. However, the infections that lead to sepsis (like the flu or pneumonia) may be transmissible.
Can you recover fully from sepsis?
Yes, many patients recover fully with early treatment. However, some may experience long-term complications like fatigue, memory issues, or organ damage.
How fast can sepsis develop?
Sepsis can develop rapidly – sometimes in a matter of hours. That’s why urgent medical attention is crucial.
📝 References :
- Tintinalli’s emergency medicine Tenth Edition
- Kumar and Clark’s clinical medicine, Tenth Edition
- Guide to the essentials in Emergency Medicine, 2nd edition
- Surviving Sepsis Campaign 2021
- https://www.ncbi.nlm.nih.gov/books/NBK430939/

