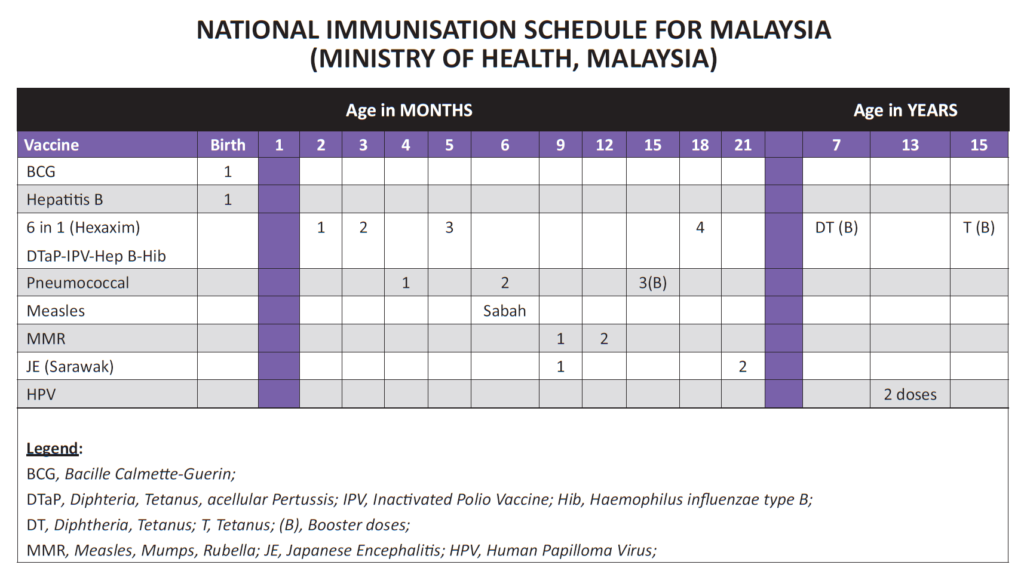
Immunizations are one of the most effective ways to protect your child from serious diseases. But with so much information out there, it can be hard to know what’s safe, what’s necessary, and when to schedule each vaccine.
In this post, we break down the key points from a comprehensive immunization guide, so you can feel confident and informed about your child’s vaccinations.
🩺 General Immunization Guidelines
Vaccines can be given at the same time without reducing effectiveness or increasing side effects. They should be administered at different injection sites unless combined into a single shot.
Sites of administration:
| Oral | Rotavirus, live typhoid vaccines |
| Intradermal (ID) | BCG (left deltoid) |
| Intramuscular (IM) | 6 in 1 DTaP-hepB-IPV-Hib (Hexaxim) |
| Deep Subcutaneous (SC): | (all vaccines except the above |
Preferred injection sites:
- Children: Anterolateral thigh
- Adults: Upper arm
- Upper outer quadrant of buttock – associated with lower antibody level production
⚠️ Contraindications: When to Delay Vaccination
- Absolute contraindication for any vaccine : severe anaphylaxis reactions to previous dose of the vaccine or to a component of the vaccine
- Acute febrile illness (postpone until recovery)
- Live vaccines: Absolute contraindications
- Immunosuppressed children – malignancy; irradiation, leukaemia, lymphoma, post-transplant, primary immunodeficiency syndromes (but NOT asymptomatic HIV): need to defer (see below)
- Pregnancy (live vaccine – theoretical risk to foetus) UNLESS there is significant exposure to serious conditions like polio or yellow fever in which case the importance of vaccination outweighs the risk to the foetus.
- Live vaccines may be given together. If not administering simultaneously then an interval ≥ 4 weeks is required.
- Tuberculin skin test (Mantoux test) and MMR: after a Mantoux test, MMR should be delayed until the skin test has been read.
- There should be ≥ 4 weeks interval for Mantoux test after MMR given.
- Killed vaccines are safe. Absolute contraindications: SEVERE local induration (involving > 2/3 of the
limbs) or severe generalised reactions in previous dose.
What is NOT a Contraindication?
- Mild illness without fever e.g. mild diarrhoea, cough, runny nose
- Asthma, eczema, hay fever, impetigo, heat rash (avoid injection in affected area)
- Treatment with antibiotics, locally acting steroids or inhaled steroids
- Child’s mother is pregnant.
- Breastfed child (does not affect polio uptake)
- Neonatal jaundice
- Underweight or malnourished
- Over the recommended age
- Past history of pertussis, measles or rubella (unless confirmed medically)
- Stable neurological conditions: cerebral palsy, mental retardation, febrile convulsions, stable epilepsy
- Family history of convulsions
- History of heart disease, acquired or congenital
- Prematurity (immunise according to schedule irrespective of gestational age)
🧬 Immunisation : Special Circumstances
Immunisation of the Immunocompromised child:
Includes malignancy; leukaemia, lymphoma, post-transplant, congenital immunodeficiency syndromes (but NOT asymptomatic HIV), immunosuppressive therapy:
- BCG is contraindicated
- Non-live vaccines can be given but may need to be repeated depending on underlying condition and
individual vaccine due to suboptimal response - For oncology patients on chemotherapy:
- Avoid live vaccines for two weeks before, during and for 6 months after completion of chemotherapy
- Safe to give influenza and pneumococcal vaccines, if indicated
- For post- Haematopoeitic Stem Cell Transplant (HSCT) and Solid Organ Transplant (SOT):
- Non-live vaccines can be given 6 months after HSCT or SOT
- Live vaccines to be given at least 2 years after HSCT and no graft versus host disease and not on immunosuppressive therapy (and acceptable CD4 count and IgM levels)
- Live vaccines contraindicated in SOT as most likely on immunosuppressive therapy
- Patients on Corticosteroid Therapy:
- On high-dose steroids i.e. Prednisolone ≥2 mg/kg/day for >14 days, delay live vaccines for at least 1 month after cessation of steroids
- On low-dose systemic steroids of 1mg/ kg/day <2 weeks or EOD for >2 weeks, can administer live vaccines
- Any dose for ≥28 days, delay live vaccines for at least 1 month after cessation of steroids.
Immunisation of children with immunomodulatory & biologics therapy
- Vaccination with non-live, attenuated vaccines in children on immunomodulation therapies and biologics is safe.
- It is recommended to withhold live-attenuated vaccines for these patients on immunomodulatory therapies and biologics. However, vaccination can be considered on a case-to-case basis weighing the benefit of vaccination against the risk of inducing infection through vaccination.
- Live-attenuated booster vaccinations against Varicella Zoster Virus and MMR can be considered in patients on low dose immunosuppressive drugs.
- For vaccination against HPV in patients with Rheumatic Diseases. Given the higher risk of HPV infection in female SLE patients, these patients should be advised to be vaccinated in the adolescence. However, physicians should be vigilant on potential thromboembolic events
Immunisation of children with HIV infection (Please refer to Paediatric HIV section)
Immunisation with Antibody-containing preparation:
- Immunoprophylaxis against viral illness provide susceptible individuals with immunologic protection against it.
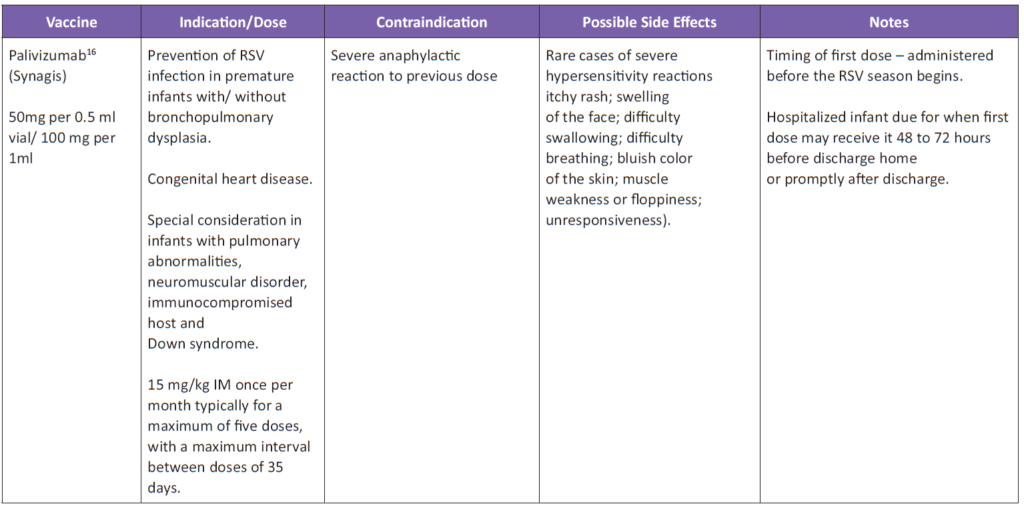
- Palivizumab is a humanized monoclonal antibody against the RSV F glycoprotein, used for the prevention of serious RSV lower respiratory tract disease in specialized group of children at high risk of RSV infection. It does not interfere with response to routine immunization with live virus vaccines (eg, measles, mumps, rubella, varicella)
Children with bleeding disorders including persistent thrombocytopenia, haemophilia or patients on anti-coagulant therapy
- Children with bleeding disorders or on long term anti-coagulant therapy may develop haematoma at intramuscular vaccine injection sites
- Thus, it is preferred to use the subcutaneous route instead of the intramuscular route
- Seek expert advice before using an alternative route.
Immunisation of Children with Egg Allergy
- Egg allergy is not a contraindication to immunization with MMR.
Measures to protect inpatients exposed to another inpatient with measles
- Protect all immunocompromised children with Immunoglobulin (NHIG) 0.25-0.5 mls/kg. (Measles may be fatal in children in remission from leukaemia)
- Check status of measles immunisation in the other children. Give measles specific Immunoglobulin, if none available to give IVIG to unimmunised children within 24 hrs of exposure. Immunisation within 72 hours aborts clinical measles in 75% of contacts.
- Discharge the inpatient child with uncomplicated measles.
- Do not forget to notify the Health Office.
Close contacts of immunodeficient children and adults
- Must be immunized, particularly against measles, polio (IPV), varicella.
Children with Asplenia (Elective or emergency splenectomy; asplenic syndromes; sickle cell anaemia) are susceptible to encapsulated bacteria and malaria.
- Pneumococcal, Meningococcal A, C, Y & W-135, Haemophilus influenza b vaccines should be given.
- For elective splenectomy (and also chemotherapy or radiotherapy): give the vaccines preferably 2 or more weeks before the procedure. However, they can be given even after the procedure.
- Penicillin prophylaxis should continue ideally for life. If not, until 16 years old for children or 5 years post splenectomy in adults.
In patients with past history or family history of febrile seizures, neurological or developmental abnormalities that would predispose to febrile seizures:
- Febrile seizures may occur 5 – 10 days after measles (or MMR) vaccination or within the first 72 hours following pertussis immunisation.
- Paracetamol prophylaxis following immunisation is not recommended.
Maternal Chicken Pox during perinatal period
(Please refer to Perinatally acquired varicella section)
In contacts of a patient with invasive Haemophilus influenzae B disease
- Immunise:
- Index case irrespective of age.
- All household, nursery or kindergarden contacts < 4 years of age.
- Chemoprophylaxis: Rifampicin at 20 mg/kg once daily (Maximum 600 mg) for 4 days (except pregnant women – give one IM dose of ceftriaxone)
- All household < 4 years who is unimmunised or incompletely immunised
- For preschool and child care facility should be at the discretion of local health department
Babies born to mothers who are Hbe Ag OR Hbs Ag positive should be given Hepatitis B immunoglobulin (200 IU) and vaccinated with the Hepatitis B vaccine within 12 hours and not later than 48 hours. Given in different syringes and at different sites
Premature infants may be immunised at the same chronological age as term infants. (Please refer The Premature Infant section).
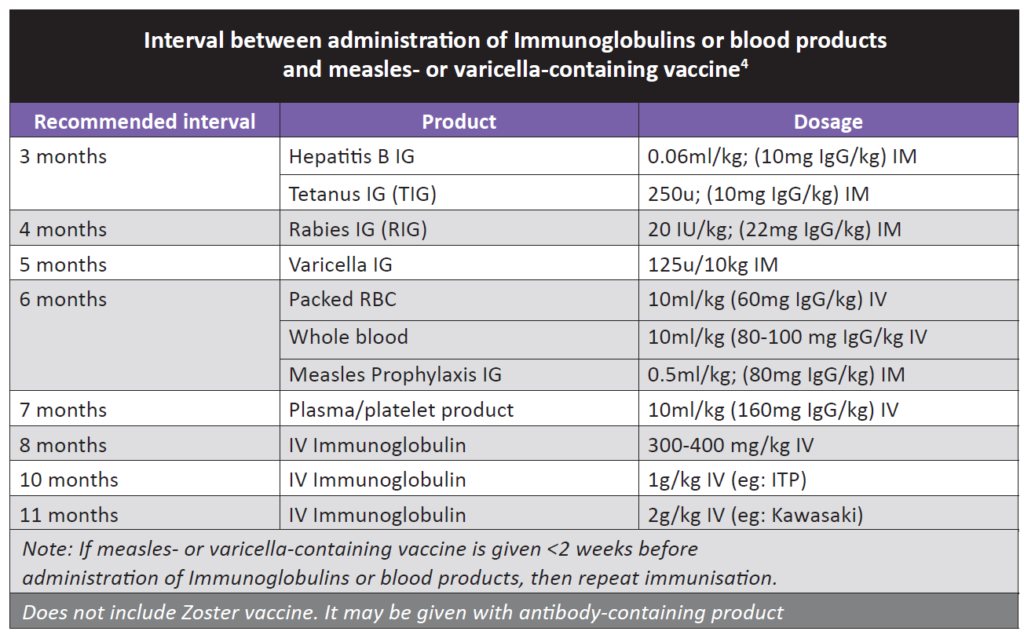
Post-Immunoglobulin or Blood Transfusion:
- Wait 3–11 months (depending on product) before giving measles or varicella vaccines
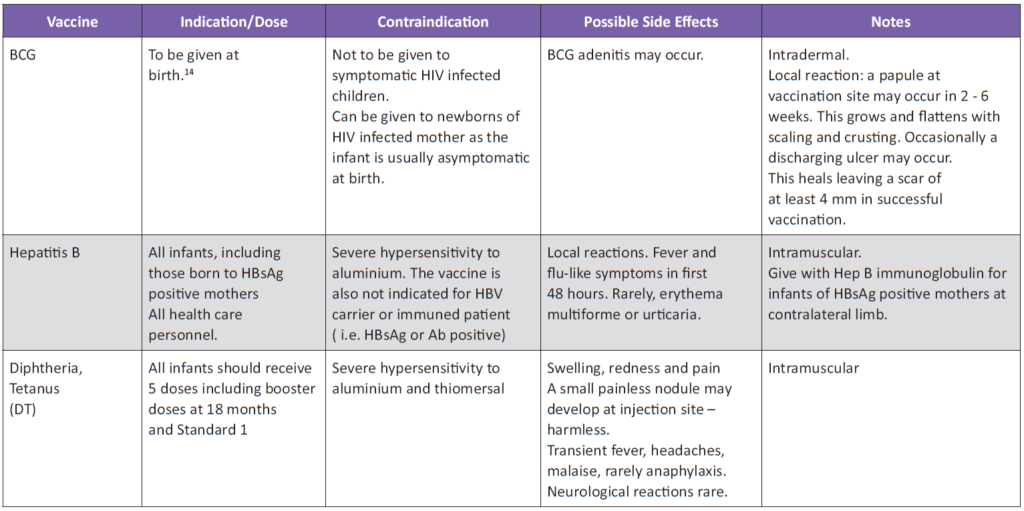
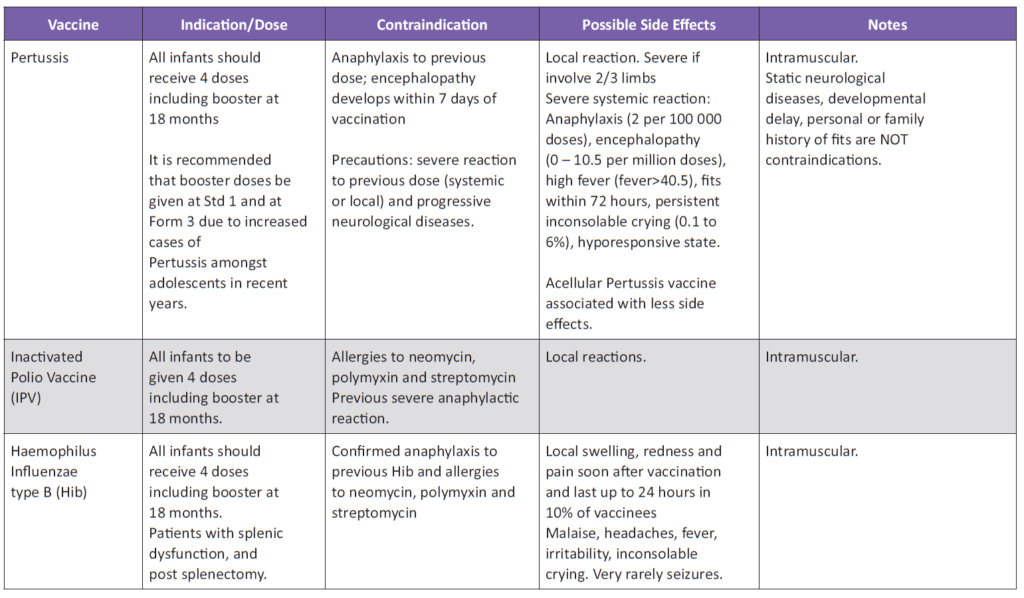
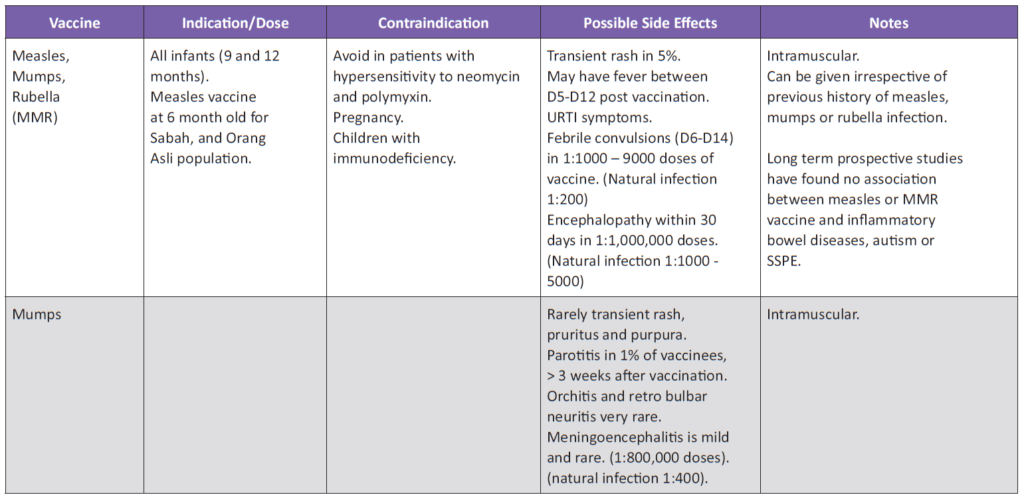
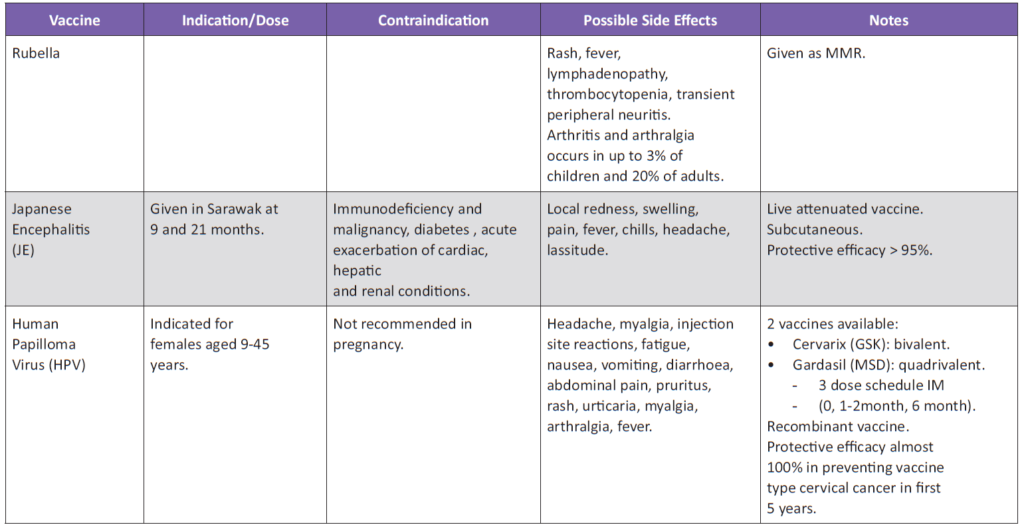
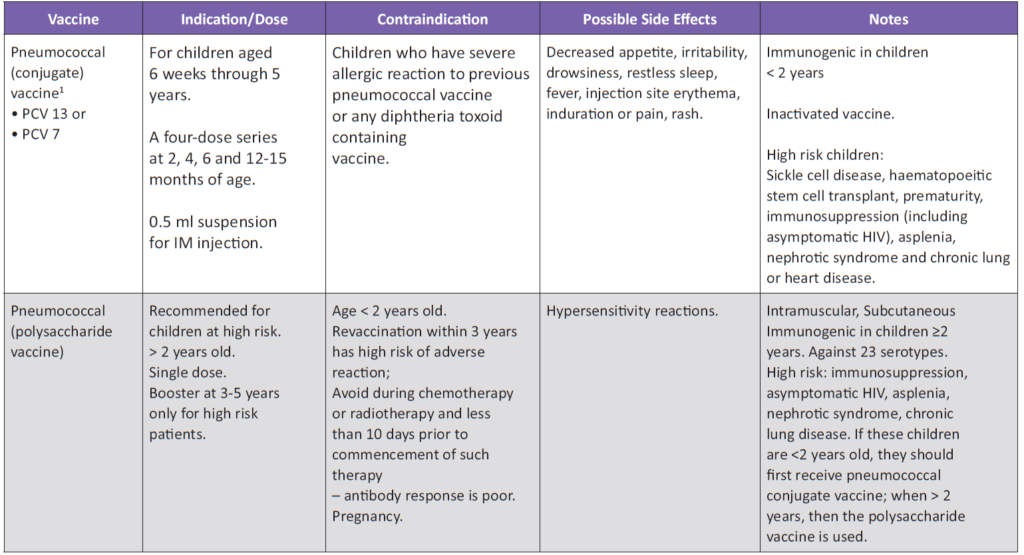
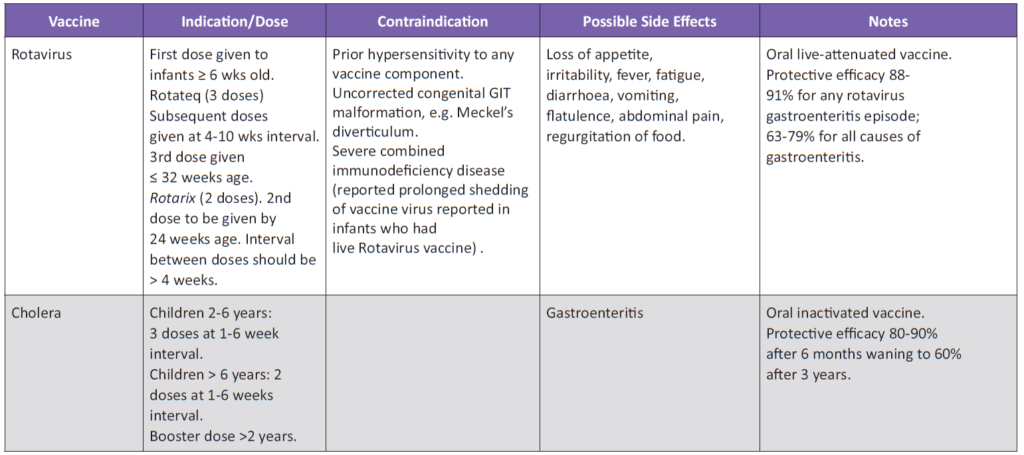
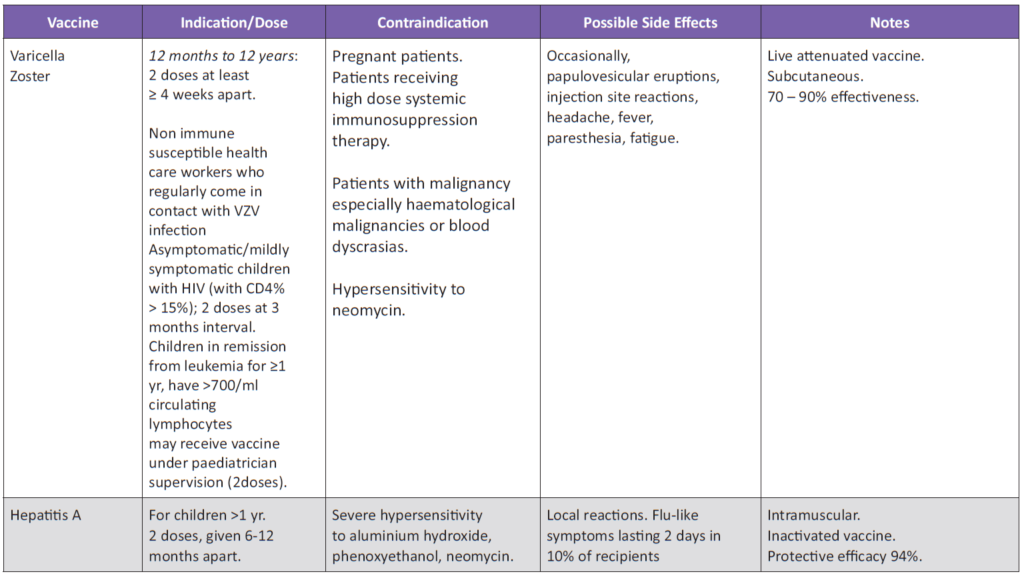
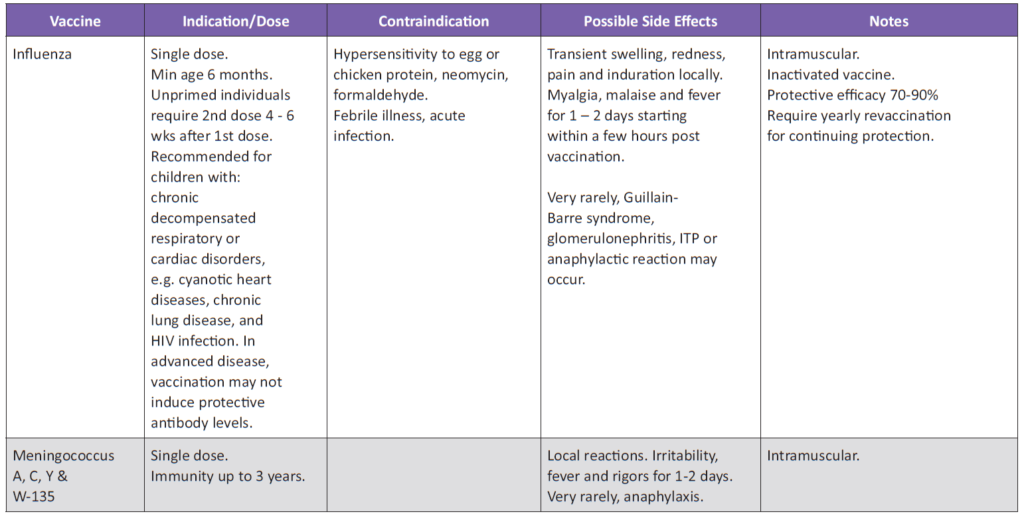
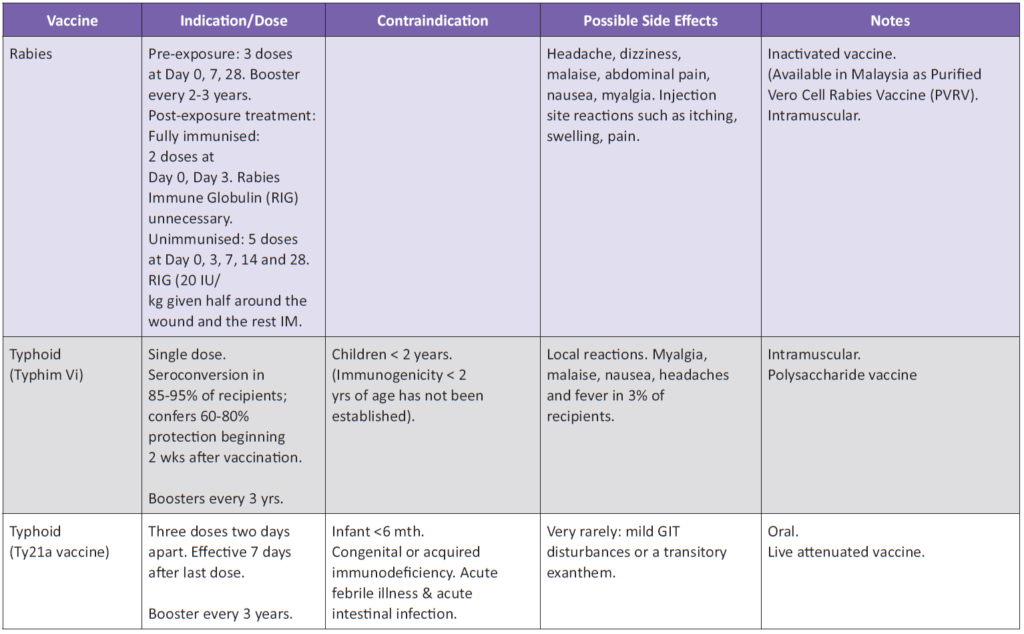
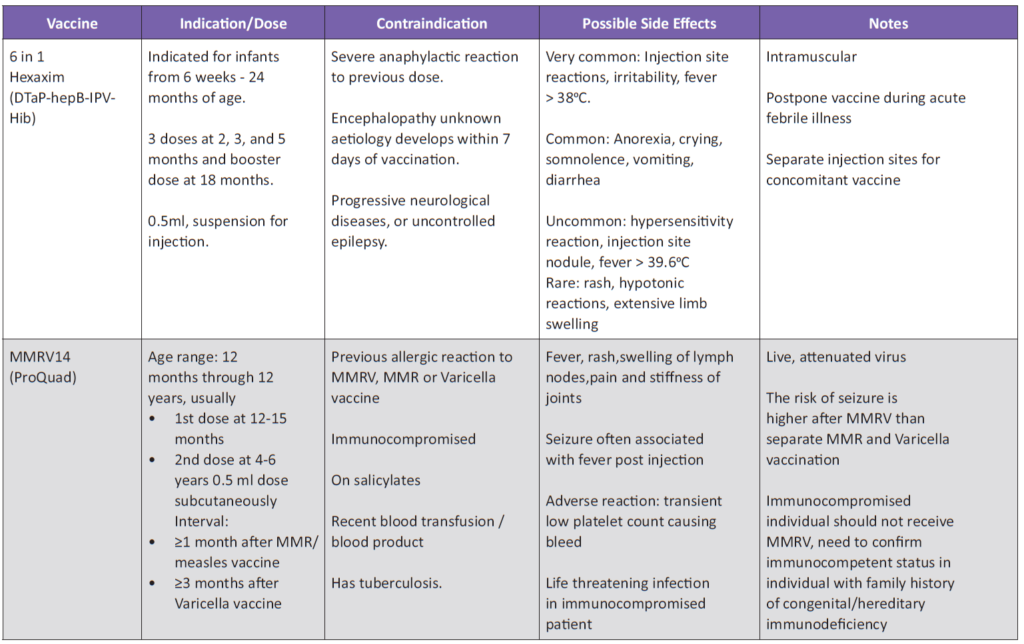
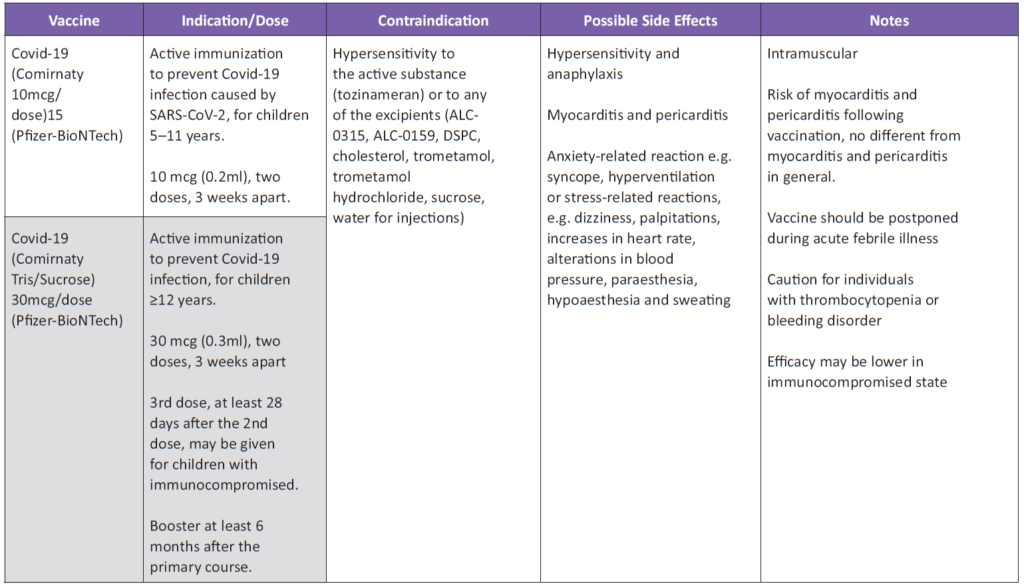
VACCINES, INDICATIONS, CONTRAINDICATIONS, DOSES AND SIDE EFFECTS
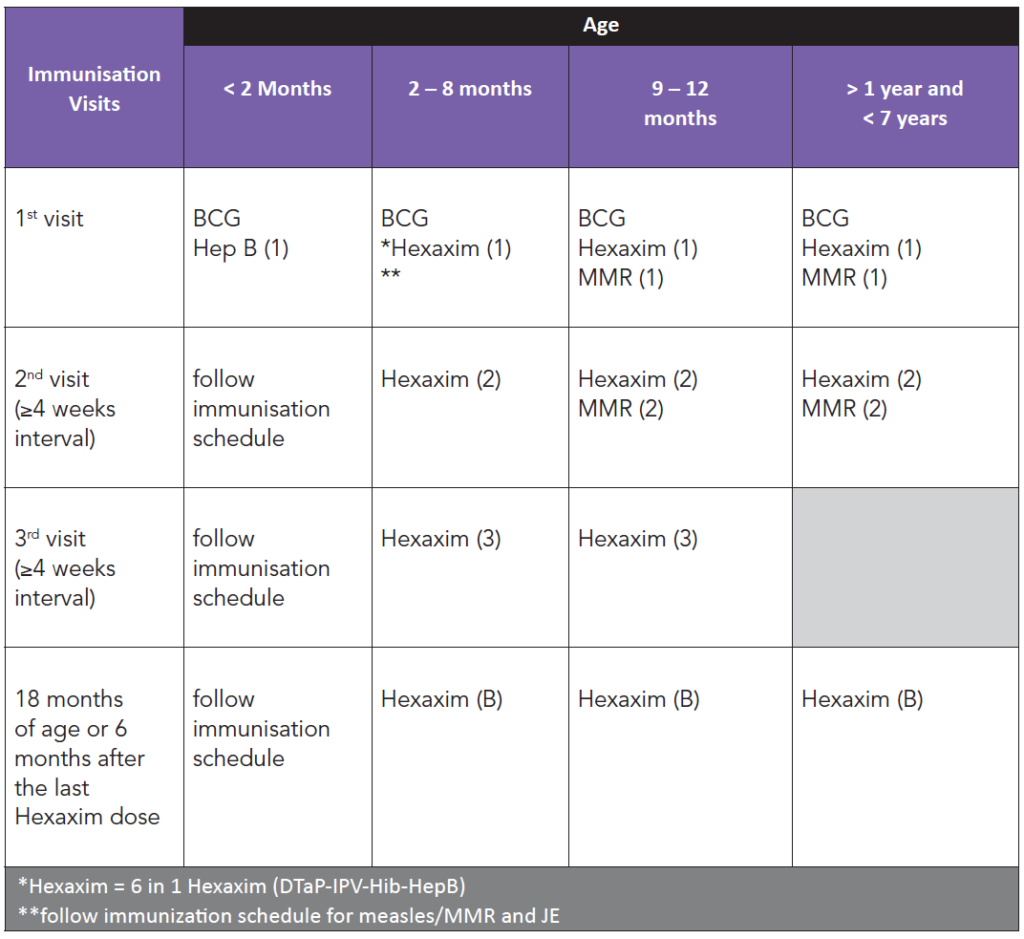
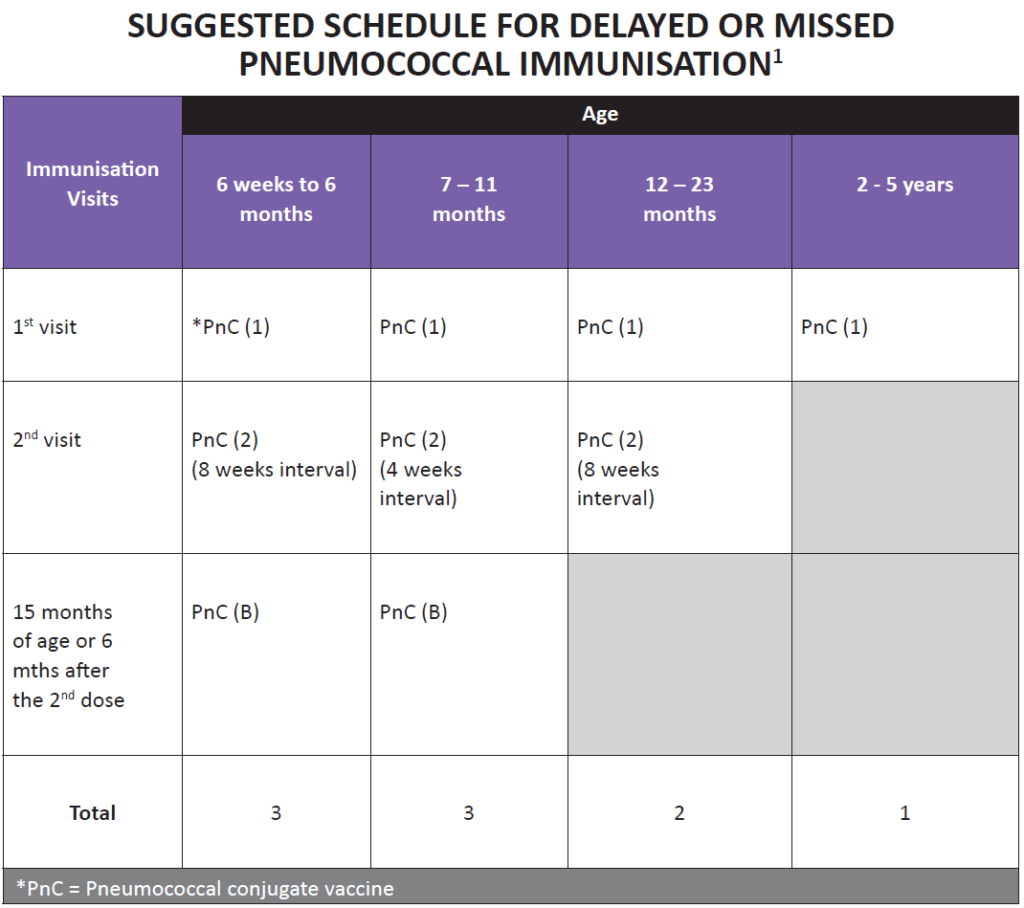
IMMUNISATION FOR CHILDREN WHO HAVE DELAYED FIRST VISIT TO THE CLINIC (NOT GIVEN IMMUNISATION)
Immunisation should be started on the first visit for children who have delayed visit to the clinic for immunisation.
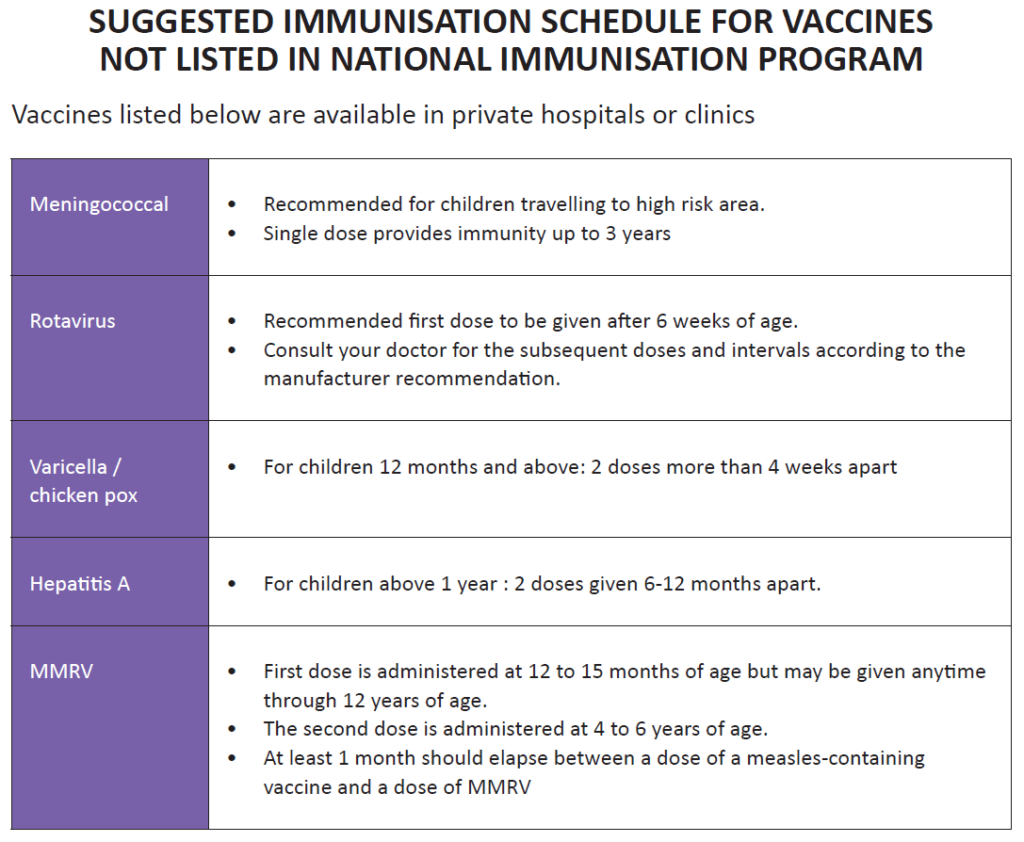
Below is the suggested schedule according to age for these children:
📌 Final Takeaways
- Vaccines are safe and can be given together.
- Mild illness is not a reason to delay.
- Special medical conditions require tailored schedules—always consult your doctor.
- Keep records of all vaccines and follow the catch-up schedule if doses are missed.
- Protect vulnerable children by ensuring family and close contacts are vaccinated.